IONM Meets Chiropractic: The Perfect Career Combination
There are worlds out there we know nothing about, but that in the end could mean the world to us. There are subjects that do not come up often that are important enough to learn about in great detail. There are widely unknown education tracks that inspire lifelong transformations. There are technologies and services that can shape the outcomes of surgeries, and there are careers that parallel your own that can make all the difference for you and others.
When we learn about new subjects, new worlds open up to us. Our eyes widen as directions change and previously unimaginable opportunities arise. When I first learned about intraoperative neuromonitoring (IONM), I found the possibilities to be as amazing as the fact that I was not aware the field even existed. I started my career after receiving a master’s degree in human nutrition from the University of Bridgeport and a doctorate from the University of Bridgeport’s School of Chiropractic. I went on to practice in the chiropractic field for nine incredible years before deciding to add IONM education to my resume.
As chiropractors, we try to treat conservatively to help avoid surgery or help to rehabilitate after the procedure. However, when surgery is necessary, it must be performed in the safest way possible to achieve the greatest possible outcome. Not unlike a surgeon, a chiropractor’s main role is to alleviate pain and improve body functions — a mission that I’ve always been passionate about. While the vast differences between the roles are obvious, there is much knowledge that the two forms of practitioners share. Both see patients with similar conditions and often refer them to specialists outside of their fields of expertise. As I prefer to take a more conservative approach, I never went so far as to pursue a career in surgery, but the medical side of healthcare has always deeply fascinated me.
After doing some research, I realized that I could grow to become more involved in medical work while continuing to be there for patients through the thriving field of IONM. By becoming a surgical neurophysiologist, I could be an advocate for patients who are under anesthesia and speak for them while they cannot speak for themselves. My experience in patient care made me a perfect candidate, and the science behind neuromonitoring even builds on the knowledge obtained during chiropractic training.
By monitoring the nervous system during surgical procedures, neurophysiologists serve as an essential layer of protection between patients and potential neurological deficits. By being present during surgeries, I am equipped to make a difference at the time of the operation. Seeing firsthand how various spinal procedures are performed, I’ve also gained a greater understanding of the type of rehabilitation patients will need after surgery.
In the end, I have found that being a surgical neurophysiologist and a chiropractor is not only more fulfilling; it also makes me a better, more well-rounded physician.
Yevgenia Boyko, DC

 Craig Crookston
Craig Crookston I have been a surgical neurophysiologist for six years, and during those six years, I have had many challenging experiences. I’m sure most SNP’s can attest to the fact that our jobs can be stressful and challenging at times but also very rewarding. This is one of those times.
I have been a surgical neurophysiologist for six years, and during those six years, I have had many challenging experiences. I’m sure most SNP’s can attest to the fact that our jobs can be stressful and challenging at times but also very rewarding. This is one of those times.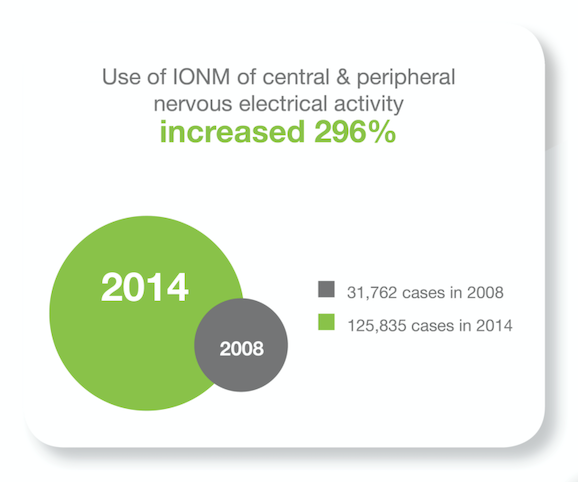 Data was collected from the National Inpatient Sample (NIS) database between 2008 and 2014 across 44 states.
Data was collected from the National Inpatient Sample (NIS) database between 2008 and 2014 across 44 states. Are you a people person? Do you like technology? Are you looking for a challenging, rewarding career in a fast-growing industry?
Are you a people person? Do you like technology? Are you looking for a challenging, rewarding career in a fast-growing industry?